Our Focus on Immuno-Oncology
In the field of immuno-oncology, the STAM™ mouse is the most pathologically suitable model for developing new therapeutic drugs for liver cancer.
The STAM™ mouse will advance your research.

Background
SMC Laboratories, Inc. is a CRO that provides non-clinical drug pharmacology study services with a focus on the liver disease area. We have developed the STAM™ mouse, the world's first mouse that induces liver cancer from MASH (metabolic dysfunction-associated steatohepatitis)/ NASH (nonalcoholic steatohepatitis). We have been providing this model for over 10 years for pharmacology studies for MASH/NASH treatment drugs.

The utilization of STAM™ mouse enables non-clinical research for the development of liver cancer therapeutics targeting immune cells, tumor microenvironment, and genetic mutations.
Advantages of STAM™ mouse in immuno-oncology.
- It can evaluate the number and localization of infiltrating cytotoxic T cells (CD8-positive T cells).
- It can evaluate the anti-tumor effects by immune checkpoint inhibitors.
- It can evaluate the assessment of tumor growth inhibiton by calculating the maximum change rate in tumor diameter of the multiple target lesions by CT.
- The tumor has high tumor mutation burden.
- It can evaluate the tumor microenvironment and its contributing factors (immunosuppressive cells, fibroblasts, immune-regulating cytokines/signal transduction, metabolic abnormalities, and gut microbiota).
The STAM™ mouse, possessing a background of late-stage type 2 diabetes, successfully reproduces the pathogenesis of human MASLD and exhibits many aspects of the pathophysiology of human MASLD and liver cancer.
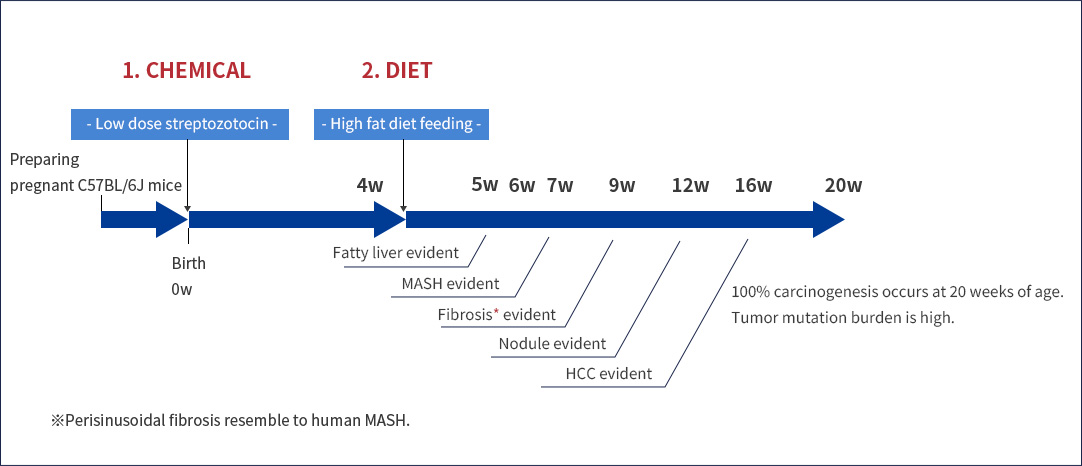
①Metabolic disorder such as hyperglycemia and hyperlipidemia
②Increase in human HCC markers: glutamine synthase, glypican-3, and AFP
③Frequent mutations in the Ctnnb1 gene, similar to human liver cancer patients. Moreover, similar mutations are observed in downstream pathways such as the Wnt pathway, cell cycle-related pathways, and chromatin modification pathways.
For all the reasons above, the STAM™ mouse can be a model that can successfully replicate clinical correlations that have not been replicated by other MASLD mouse models, such as the GAN diet model or MS-NASH model.

The STAM™ mouse has been reported as the most suitable mouse model for liver cancer according to Dow et al. from the University of California, San Diego.
The STAM™ mouse can help you advance your research.

Key publications
Genentech, December 2018
Transcriptomic analysis of hepatocellular carcinoma reveals molecular features of disease progression and tumor immune biology
Figure 1
ARTICLE OPEN
Transcriptomic analysis of hepatocellular carcinoma reveals
molecular features of disease progression and tumor immune biology
K Okrah # 1, S Tarighat # 2, B Liu # 2, H Koeppen 3, M C Wagle 2, G Cheng 2, C Sun 2, A Dey 4, M T Chang 4, T Sumiyoshi 2, Z Mounir 2, C Cummings 2, G Hampton 2, L Amler 2, J Fridlyand 1, P S Hegde 2, S J Turley 4, M R Lackner 2, S M Huang 2
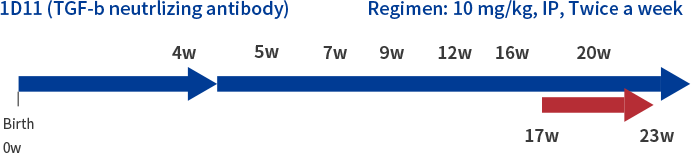
Regarding the therapeutic effects on liver cancer, Okrah et al from Genentech have reported the potential of suppressing liver cancer through the administration of a stroma-modifying drug (TGF-β neutralizing antibody, 1D11 antibody), which improves fibrosis in the tumor microenvironment. Administering the TGF-β neutralizing antibody to STAM™ mice in the liver cancer phase has been shown to decrease fibrotic areas, reduce the number and diameter of tumors in the liver, and increase the infiltration of CD8+ T cells into the tumors. This suggests therapeutic effects on liver cancer through changes in T cell localization mediated by the improvement of fibrosis (see Figure 1). The effectiveness of immune checkpoint inhibitors used in clinical settings has been reported to depend significantly on the tumor microenvironment. Targeting the immunosuppressive tumor microenvironment is believed to bring a new breakthrough in the research of liver cancer therapeutics.
Example studies
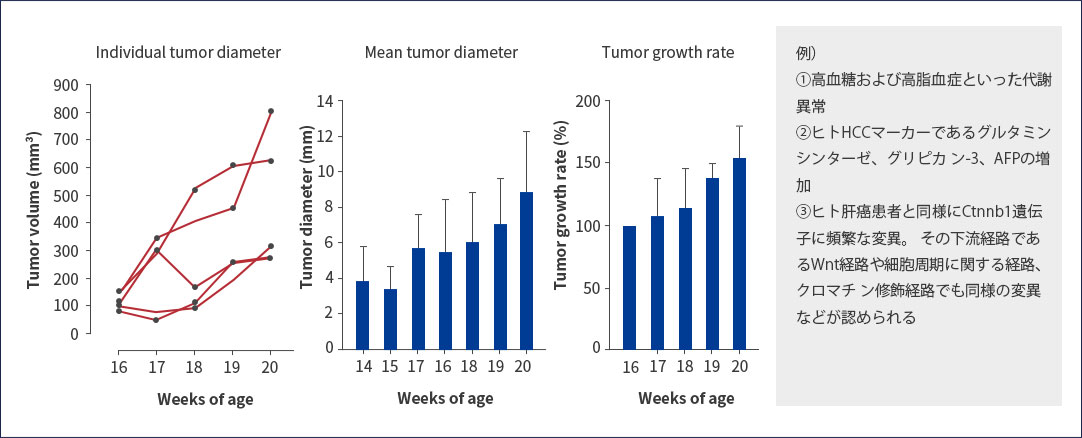
The anti-PD-L1 antibody (clone: 10F.9G2) used in clinical practice demonstrated a tumor growth inhibition at the rate of 75.1% in liver cancer treatment trials using STAM™ mice, with observed tumor shrinkage effects (see Figure 2).
Figure 2
PD-L1mAb (10F.9G2)
【Regimen: 5 mg/kg, IP, Twice a week】
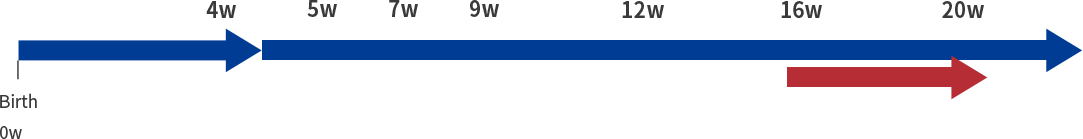
Relative tumor volume and tumor growth inhibition are calculated by following formula;
Relative tumor volume (%) = tumor volume at 20 weeks of age/ tumor volume at 16 weeks of age.
Tumor growth inhibition (%) = (RTV average of Isotype group - RTV average of PD-L1 group)/ RTV average of Isotype group x 100%
Tumor growth inhibition
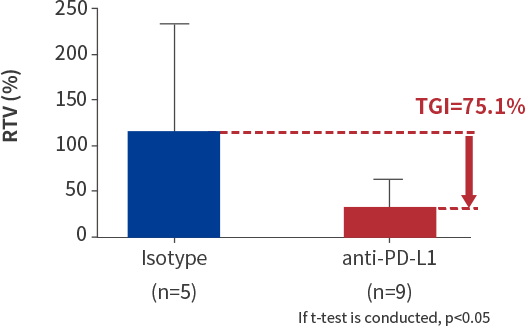
Anti-PD-L1 antibody, an immune checkpoint inhibitor, suppresses tumor growth inhibition (*Tumor growth inhibition is calculated using the relative tumor volume).
As in this case, the STAM™ model shows immune responses and is capable of evaluating ICIs.
In this way, the STAM™ mouse is currently the only model that allows the efficacy evaluation on tumors not only for immunotherapy with immune checkpoint inhibitors, but also for stroma-modifying drugs that alter the tumor microenvironment.
Table 1. A summary of molecular targets in the tumor immune microenvironment of hepatocellular carcinoma
| Target cell | Molecule | Major effects | Therapeutic strategy |
|---|---|---|---|
| MDSC | CCL26 | CCL26 mediates MDSC recruitment in the hypoxic regions of HCC. | CCL26 blockade |
| CCL9/CCR1 | CCL9/CCR1 induces MDSCs recruitment to the spleen. | CCL9/CCR1 blockade | |
| ENTPD2/CD39L1 | HIF-1 prompts MDSC accumulation via ENTPD2/CD39L1 in HCC. | ENTPD2/CD39L1 blockade |
|
| CCRK | CCRK induction drives mTORC1-dependent G-CSF expression to recruit MDSCs and enhance tumorigenicity in HCC. | Anti-CCRK | |
| IL-6 | IL-6 expression level is highly associated with MDSC phenotype in HCC patients. | Anti-IL-6 | |
| PD-L1 | PD-L1+ MDSCs area increased in HCC patients. | PD-L1 blockade | |
| C5AR | C5AR can recruit MDSCs to the TIME. | C5AR blockade | |
| Treg | PD-1 | PD-1-mediated inhibitory signal in the TME. | PD-1 blockade |
| CTLA-4 | Tumor-induced regulatory DC subset inhibit immunity via CTLA-4-dependent IL-10 and IDO production. | CTLA-4 blockade | |
| TIM3 | Antibodies against TIM3 restore immune response of HCC-derived T cells to tumor-specific antigens. | TIM3 blockade | |
| LAG3 | Antibodies against LAG3 restore immune response of HCC-derived T cells to tumor-specific antigens. | LAG3 blockade | |
| GITR | GITR-ligation can improve anti-tumor response by abrogating Treg-mediated suppression in HCC | GITR blockade | |
| ICOS | ICOS+FOXP3+ Treg cells are enriched in the HCC TME | ICOS blockade | |
| CCR4 | Tregs can be targeted and depleted by mABs towards CCR4. | Anti-CCR4 | |
| TGF-β TGF-β prompts Treg infiltration into the liver. Sorafenib | TGF-β prompts Treg infiltration into the liver. | Sorafenib | |
| TAM | IL-6, IL-23, IL-β, TNF-α | Cytokines enhance the expansion of IL-17-producting CD4+Th17 cells. | Anti-IL-6, anti-IL-23, anti-IL-β, anti-TNF-α |
| TGF-β | TGF-β prompts TIM-3 expression in TAMs. | Anti-TGF-β | |
| IL-1β | IL-1β prompts EMT and HCC immune escape. | Anti-IL-1β | |
| CCR2 | CCR2 prompts EMT transition and M2-plarization of TAMs | Anti-CCR2 | |
| CSF-1 | CSF-1 reprograms polarization of TAMs | CSF-1 receptor antagonist |

The STAM™ mouse is currently the only model that allows the evaluation of the effects on tumors not only for immunotherapy, centered around immune checkpoint inhibitors, but also for therapeutics that modify the tumor microenvironment.
The STAM™ mouse can help you advance your research.
References
- Huang DQ et al,: Global epidemiology of NAFLD-related HCC: trends, predictions, rick factors and prevention, Nature Reviews Gastroenterology & Hepatology, vol 18, 223-238 (2021)
- Chen C et al,: Tumor microenvironment-mediated immune evasion in hepatocellular carcinoma, frontiers inImmunology, vol 14, 1133308 (2023)
- Tan S et al,: Immune checkpoint inhibitor therapy in oncology: current uses and future directions, JACC: CardioOncology, vol 4, 579-597 (2022)
- Valero C et al,: Inappropriate use of the same cutoff by different sequencing panels for tumor mutation burdenas immunotherapy biomarker, JAMA Oncology, 7, 1245-1246 (2021)
- Fujii M et al,: A murine model for non-alcoholic steatohepatitis showing evidence of association betweendiabetes and hepatocellular carcinoma, Medical Molecular Morphology, vol. 46, 141-152 (2013).
- Takakura K et al,: Characterization of non-alcoholic steatohepatitis-derived hepatocellular carcinoma as ahuman stratification model in mice, Anticancer Research, vol.34, 4849-4855 (2014).
- Dow M et al,: Integrative genomic analysis of mouse and human hepatocellular carcinoma, PNAS, vol 115,E9879-E9888 (2018).
- Li E et al,: Mouse models for immunotherapy in hepatocellular carcinoma, Cancers, vol 11, 1800 (2019)
- Bresnahan E et al,: Mouse models of oncoimmunology in hepatocellular carcinoma, Clinical Cancer Research,vol 26, 5276-5286 (2020)
- Okrah K et al,: Transcriptomic analysis of hepatocellular carcinoma reveals molecular features of diseaseprogression and tumor immune biology, NPJ Precision Oncology, vol 25 (2018).
Current status of liver cancer
- The 4th most common cancer in the world
- 3rd leading cause of cancer-related deaths

Cause of liver cancer development
Various factors like B type/C type hepatitis, consumption of alcohols, diabetes and MASH/NASH.

Among them, the proportion of non-B/non-C type cancer like MASH/NASH, which is not associated with viral hepatitis is increasing year by year.
Treatment drugs and response rates for liver cancer
In addition to molecular targeted drugs such as lenvatinib and sorafenib, immune checkpoint inhibitors like atezolizumab + bevacizumab, nivolumab, and pembrolizumab have been used in clinical practice in recent years.
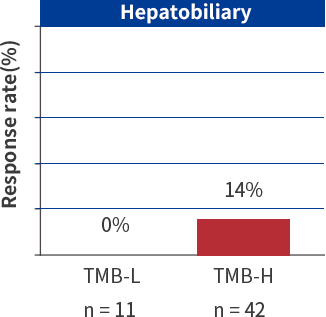
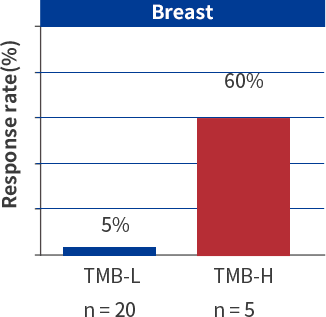
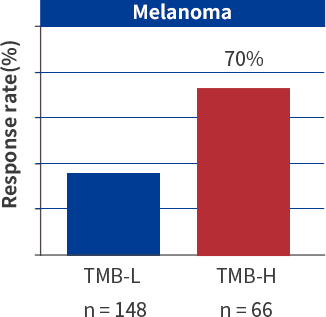
Immune checkpoint inhibitors and response rate for various cancer
The response rate of immune checkpoint inhibitors for liver cancer is between 0-14%, which is lower compared to other cancers (for example, the response rate for melanoma is 35-70%). Due to this, there is an expectation for the development of novel therapeutic drugs. Additionally, there are many challenges in the models of mice used in the field of immuno-oncology, including a lack of diversity and heterogeneity in cancer cell lines, tumors not originating from normal cells, and the failure to reproduce the tumor microenvironment (see Table 2).
Table 2. Mouse models for immuno-oncology in hepatocellular carcinoma
| Model | STAMTM | DEN | CDAHFD | Syngeneic implantation; orthotopic |
Syngeneic implantation; subcutaneous |
Xenograft; orthotopic |
Xenograft; subcutaneous |
|---|---|---|---|---|---|---|---|
| Background | Diabetic/ Inflammation/ fibrosis |
Fibrosis | Diabetic/ Inflammation/ fibrosis |
Normal liver | Normal skin | Normal liver | Normal skin |
| Inducer | Chemical / Diet (STZ / HFD) |
Chemical (Diethylnitrosamine) |
Diet | Mouse HCC cell line (HCA-1, RIL-175, Hepa1-6) |
Mouse HCC cell line(RIL-175, BNL-1MEA) | Human HCC cell line(HepG2, Hep3B, SK-Hep1, Huh7) | Human HCC cell line(HepG2, Hep3B, SK-Hep1, Huh7) |
| Host strain | C57BL/6J | C57BL/6J | C57BL/6J | C3H, C57BL/6, BALB/c | C57BL/6, BALB/c | Nude, SCID | Nude, SCID |
| Time to develop tumors | 16-20 wks | 45-102 wks | 36 wks | 1-2 wks | 1-2 wks | 1-2 wks | 1-2 wks |
| % of mice with HCC | 100% (20 wks) | 80-100% | 27% (at 60 wks) | 100% | 100% | 100% | 100% |
| Development of therapeutic drugs for tumor microenvironment |
|
Not reported | Not reported | Not reported* |
|
Not reported |
|
| Development of therapeutic drugs for immune checkpoint inhibitor |
|
Not reported |
|
|
|
|
|
| Remarks | Tumor mutation burden-high | Genetic mutations are not similar to human HCC | There are no reports of peri-tumoral and intratumoral T cell localization. | Lack of diverse cancer cell line and heterogeneity | Unable to analyze tumor microenvironment | Immune cell deficiency | Immune cell deficiency |
*We searched for literature in PubMed using the keyword “syngeneic orthotopic”, “tumor microenvironment”, “HCC”, “stromal modifying agent”, but no literature was found as of October 2023.

There has been high anticipation for the development of new therapeutic drugs for liver cancer.
In response to this social background, we provide clinical efficacy evaluation services for novel hepatocellular carcinoma drugs, including immune checkpoint inhibitors, by utilizing various advantageous characteristics of STAM™ mouse, which develop hepatocarcinoma in a short period of time.
The STAM™ mouse can help you advance your research.